Why Cholesterol is Essential for Optimal Health, and the Six Most Important Risk Factors of Heart Disease
December 30, 2012 | 105,704 views | + Add to Favorites
| 690 |
|
Print
|
Click HERE to watch the full interview!
Download Interview Transcript
Visit the Mercola Video Library
By Dr. Mercola
There's some serious confusion about cholesterol, and whether high cholesterol levels are responsible for heart disease.
Chris Masterjohn, who recently received his PhD in nutritional sciences from the University of Connecticut, has published five peer-reviewed papers on vitamins and supplementation, and he's currently researching fat-soluble supplements – A, D, and K – at the University of Illinois. (Please note that the opinions expressed here represent Dr. Masterjohn's own positions, and may not represent the position of the University of Illinois.)
He also maintains a blog, The Daily Lipid1, and his website, Cholesterol-And-Health.com2, which are dedicated to the issue of cholesterol. He's also active with the Weston A. Price Foundation.
Cholesterol has been demonized since the early 1950's, following the popularization of Ancel Keys' flawed research. As a result, people now spend tens of billions of dollars on cholesterol-reducing drugs each year, thinking they have to lower this "dangerous" molecule lest they keel over from a heart attack.
As a testament to the power of this incredibly effective marketing system, Lipitor was the number one selling drug for 2011. This also reveals why challenging this belief system is met by such intense resistance. There are very powerful, financially-motivated forces backing the continued belief in the cholesterol myth.
Cholesterol is Essential for a Healthy Life
The Weston A. Price Foundation has been a major leader in helping people understand the truth about cholesterol, and Dr. Masterjohn has also lectured on this important topic.
"If we want to understand why cholesterol is really an incredibly important molecule and is really our friend rather than our enemy, I think what we should look at is the question, "What happens without cholesterol?" he says.In those rare cases where a baby is born with Smith-Lemli-Opitz syndrome, the child is susceptible to and can present a wide range of defects, such as:
... [L]ook at Smith-Lemli-Opitz syndrome or SLOS, which is a symptom of genetic deficiency in cholesterol. It's when people can't make enough cholesterol on their own. In order to actually have this full-blown syndrome, it's a recessive trait, which means you need a defective gene for cholesterol synthesis from your father, and you need one from your mother as well. Now, the number of people who carry this defective gene in the population is about one to three percent of the population. However, the number of babies who are born with Smith-Lemli-Opitz syndrome is far lower than we would expect.
... It turns out that if [the fetus] has both of these genes and the unborn child can't synthesize its own cholesterol, then this usually results in spontaneous abortion. So right away we see that cholesterol is needed for life itself..."
Autism or mental retardation Failure to thrive Physical defects in hands, feet and/or internal organs Visual problems Increased susceptibility to infection Digestive problems
Cholesterol is Essential for Cellular Function
What this tells us is that cholesterol deficiency impacts virtually every aspect of your health. One of the primary reasons for this widespread effect is because cholesterol plays a critical role within your cell membranes. Your body is composed of trillions of cells that need to interact with each other. Cholesterol is one of the molecules that allow for these interactions to take place. For example, cholesterol is the precursor to bile acids, so without sufficient amounts of cholesterol, your digestive system can be adversely affected.
It also plays an essential role in your brain, which contains about 25 percent of the cholesterol in your body. It is critical for synapse formation, i.e. the connections between your neurons, which allow you to think, learn new things, and form memories. In fact, there's reason to believe that low-fat diets and/or cholesterol-lowering drugs may cause or contribute to Alzheimer's disease3. Low cholesterol levels have also been linked to violent behavior, due to adverse changes in brain chemistry.
Furthermore, you need cholesterol to produce steroid hormones, including your sex hormones. Vitamin D is also synthesized from a close relative of cholesterol: 7-dehydrocholesterol.
To further reinforce the importance of cholesterol, I want to remind you of the work of Dr. Stephanie Seneff, who also works with the Weston A. Price Foundation. One of her theories is that cholesterol combines with sulfur to form cholesterol sulfate, and that this cholesterol sulfate helps thin your blood by serving as a reservoir for the electron donations you receive when walking barefoot on the earth (also called grounding). She believes that, via this blood-thinning mechanism, cholesterol sulfate may provide natural protection against heart disease. In fact, she goes so far as to hypothesize that heart disease is likely the result of cholesterol deficiency — which of course is the complete opposite of the conventional view.
Identifying Risk Factors for Heart Disease
Heart disease is clearly one of the leading causes of death in the US, making it imperative for the vast majority of people to understand the risk factors in order to avoid becoming a statistic. However, total cholesterol will tell you virtually nothing about your disease risk, unless it's exceptionally elevated (above 330 or so, which would be suggestive of familial hypercholesterolemia, which, in my view, would be about the only time a cholesterol-reducing drug would be appropriate).
Two ratios that are far better indicators of heart disease risk are:
Four additional risk factors for heart disease are:
- Your HDL/total cholesterol ratio: HDL percentage is a very potent heart disease risk factor. Just divide your HDL level by your total cholesterol. This percentage should ideally be above 24 percent. Below 10 percent, it's a significant indicator of risk for heart disease
- Your triglyceride/HDL ratios: This percentage should ideally be below 2
- Your fasting insulin level: Any meal or snack high in carbohydrates like fructose and refined grains generates a rapid rise in blood glucose and then insulin to compensate for the rise in blood sugar. The insulin released from eating too many carbs promotes fat and makes it more difficult for your body to shed excess weight, and excess fat, particularly around your belly, is one of the major contributors to heart disease
- Your fasting blood sugar level: Studies have shown that people with a fasting blood sugar level of 100-125 mg/dl had a nearly 300 percent increase higher risk of having coronary heart disease than people with a level below 79 mg/dl
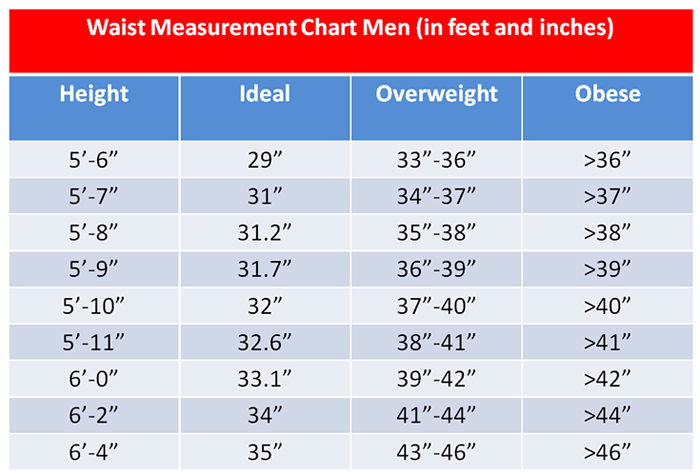
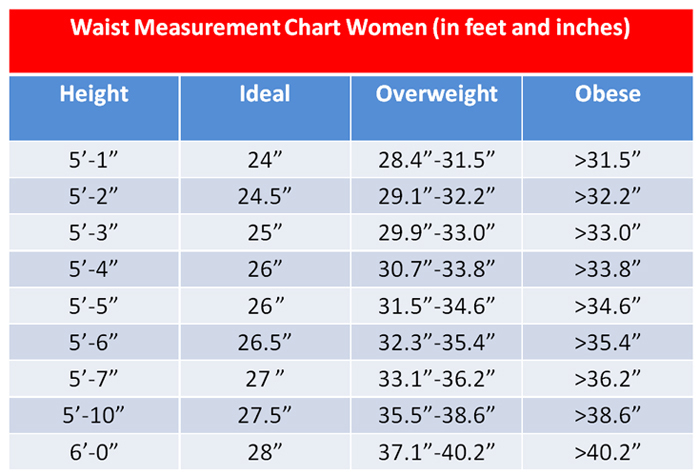
- Your waist circumference: Visceral fat, the type of fat that collects around your internal organs, is a well-recognized risk factor for heart disease. The simplest way to evaluate your risk here is by simply measuring your waist circumference. For further instructions, please see my previous article, Your Waist Size Can Be a Powerful Predictor of Hypertension and Other Chronic Diseases
- Your iron level: Iron can be a very potent oxidative stress, so if you have excess iron levels you can damage your blood vessels and increase your risk of heart disease. Ideally, you should monitor your ferritin levels and make sure they are not much above 80 ng/ml. The simplest way to lower them if they are elevated is to donate your blood. If that is not possible you can have a therapeutic phlebotomy and that will effectively eliminate the excess iron from your body
What You Need to Know about LDL and HDL with Respect to Heart Disease
LDL and HDL stand for low-density lipoprotein and high-density lipoprotein respectively. While most people talk about them as if they're different types of cholesterol, these lipoproteins are actually carriers for cholesterol in the blood. According to Dr. Masterjohn:
"I think there's some truth to this basic paradigm in terms of their predictive value and the ability of LDL and HDL cholesterol to let us know whether things need to be optimized in the body. But I think it's important to note that just because these markers tend to correlate with [heart disease] risk, does not mean that one thing is causing the other.According to Dr. Masterjohn, the researchers claim this failure was not related to the specific function of the drug, but rather that it had "off-target toxicity" that ended up putting people in mortal danger. He mentions another drug, Anacetrapib, which does the same thing as the failed Torcetrapib. So far, the short-term results have been promising, but the short-term results for Torcetrapib had also seemed promising, so I join him in issuing a warning well ahead of time that this drug — if released — is probably going to have some pretty significant detrimental side effects...
For example, one of the most powerful predictors that's been validated across dozens of studies using hundreds of thousands of people is the total cholesterol to HDL cholesterol ratio... Basically, the higher the total to HDL cholesterol ratio, the greater the risk of future heart disease.
Now, does this mean that a high total to HDL cholesterol ratio causes heart disease?
Well, the best way to put that to the test would be to come up with a drug that specifically changes the ratio of LDL to HDL cholesterol ratio and to see if that drug prevents heart disease.
So far, they've tried to do studies on this, which have been miserable failures. The most famous of these was the trials with Torcetrapib, which inhibited the enzyme that transfers cholesterol from HDL to LDL. By doing so, it specifically increased HDL cholesterol and decreased LDL cholesterol. But what happened? People started dying left and right after taking that drug. They had to cancel [the study] early."
Proper LDL Turnover is Important for Prevention of Heart Disease
Dr. Masterjohn points out that just because the total to HDL cholesterol ratio predicts heart disease doesn't mean that it causes heart disease.
"We need to be really careful and keep that in mind, because the same thing applies to any other marker we look at," he says. My personal view is this: these lipoproteins need to transport cholesterol through your body so that the cholesterol can be used for all the good things that cholesterol does... bile acids... sex hormones... all these great things. In order to do that, we need to have good metabolism and good turnover of LDL particles. We have a receptor called the LDL receptor. And the function of that receptor is to bring those lipoproteins into the cell, so that they can be used for all those good things."There are two primary governors of LDL receptor activity:
According to Dr. Masterjohn, when the total cholesterol to HDL cholesterol ratio increases, it may indicate poor LDL turnover and poor metabolism of the cholesterol, meaning your body is not using the available cholesterol appropriately. When your cells are not metabolizing cholesterol properly, the LDL carrier particles will stick around in your circulatory system longer, placing them at greater risk for oxidation and damage. And that's when the LDL particles become harmful.
- Individual cells: Individual cells retrieve needed cholesterol by taking in LDL particles from your blood
- Thyroid hormone
"When those particles are damaged, then they become toxic to the cells in that line of blood vessels. The immune system comes along and cleans up those damaged particles by creating a plaque," he explains.Now, as just mentioned, thyroid hormone is a communication molecule that helps govern LDL receptor activity. So when your thyroid hormone is not working properly, your LDL receptor activity will also be affected. Thyroid hormone, in turn, is governed in part by insulin. Insulin may even have a direct impact on promoting LDL receptor activity, according to Dr. Masterjohn.
"Insulin helps us make more thyroid hormone, and it helps activate T4 into T3. This helps increase LDL receptor activity and turn over these LDL particles. The problem is that a huge portion of our population is insulin-resistant. The insulin is there (maybe even more insulin than usual is there), but it's not carrying out its function properly.I've long stated that insulin resistance is at the root of virtually every chronic disease known to man, and this again strengthens my position that normalizing your insulin sensitivity should be your top priority if you seek to stop or reverse the progression of any disease process, or to optimize your health and prevent disease in the first place.
I think correcting insulin resistance is probably a major factor in normalizing thyroid function, which in turn could normalize cholesterol metabolism," he says.
The Importance of Vitamin K2 for Heart Health
There's another important contributor to a healthy vascular system and that's vitamin K2, which is responsible for the integration of calcium into arterial plaque caused by oxidized LDL particles. It's critical for keeping your arteries squeaky clean, and works in conjunction with a number of other nutrients, most important of which are vitamin D, calcium and magnesium.
Vitamin K2 is found primarily in fermented foods and animal fats. The best sources of it that most people consume are egg yolks and cheese, especially hard cheeses.
"We have epidemiological evidence that the more vitamin K2 people eat – but not K1 – the lower their risk of heart disease, and the lower their risk of calcification of the heart valves," Dr. Masterjohn says. "We also have a lot of evidence from animal experiments showing that vitamin K2 is important in protecting against calcification of the blood vessels in general.According to Dr. Masterjohn, animal studies have shown you can likely reverse arterial calcification with high doses of vitamin K2. This would not surprise me in the least, especially if you also optimize other nutritional variables that we know tend to normalize your cholesterol profiles, such as increasing consumption of healthful fats and restricting your intake of vegetable oils.
Calcification basically occurs in two ways in the blood vessels, and both of them we need vitamin K to protect against. In both cases, wherever we find the calcification, we find defective matrix Gla protein or MGP. MGP is a vitamin K-dependent protein responsible for protecting blood vessels and other soft tissues from calcification. If vitamin K is not present in sufficient quantities in the diet, it cannot activate MGP, so MGP is defective and MGP therefore cannot protect against calcification of the blood vessels, heart valves, and all their soft tissues.
It seems from the evidence that we have that insufficient intake of vitamin K2 leads to greater calcification in atherosclerosis and greater medial calcification, which in turn increases the risk for heart disease. This is particularly ironic, because in most people's diet, the best sources are eggs and cheese, which are high in cholesterol, which we're told to avoid."
Are You Getting Enough Vitamin K2 to Protect Your Heart?
The optimal amounts of vitamin K2 are still under investigation, but it seems likely that 180 to 200 micrograms of vitamin K2 should be enough to activate your body's K2-dependent proteins to shuttle the calcium where it needs to be, and remove it from the places where it shouldn't.
As I've discussed on numerous occasions, vitamin D is a critical nutrient for optimal health and is best obtained from sun exposure or a safe tanning bed. However, many are taking oral vitamin D, which can actually be problematic unless you're also getting sufficient amounts of vitamin K2. In fact, this is a really crucial point that has not been emphasized enough in the past: If you opt for oral vitamin D, you need to also consume in your food or take supplemental vitamin K2.
Why?
Because when you take vitamin D, your body creates more vitamin K2-dependent proteins — the proteins that help move the calcium around in your body. But you need vitamin K2 to activate those proteins. If they're not activated, the calcium in your body will not be properly distributed and can lead to weaker bones and hardened arteries.
In short, vitamin K2 ensures the calcium is deposited and removed from the appropriate areas. By taking vitamin D, you're creating an increased demand for K2. And vitamin D and K2 work together to strengthen your bones and improve your heart health.
My favorite source of vitamin K2 is fermented vegetables made with a special starter culture designed to cultivate vitamin K2-producing bacteria. We recently had samples of high-quality fermented organic vegetables made with our specific starter culture tested, and were shocked to discover that not only does a typical serving of about two to three ounces contain about 10 trillion beneficial bacteria, but it also contained 500 mcg of vitamin K2.
Please note that not every strain of bacteria makes K2. For example, most yogurts have almost no vitamin K2. Certain types of cheeses are very high in K2, and others are not. It really depends on the specific bacteria. You can't assume that any fermented food will be high in K2, but some fermented foods are very high in K2, such as natto.
|
|
|
Print
|


No comments:
Post a Comment