“Legalization and decriminalization is happening at a decent pace, but we can’t wait around for the government to do it… on their corporate-serving terms.” ~ Wes Annac
Sunday, December 31, 2017
Saturday, December 30, 2017
Still Believe Nature Got It Wrong? Top 10 Health Benefits of Marijuana
 By Marco Torres
By Marco Torres
Guest writer for Wake Up World
There is no plant on Earth more condemned than marijuana. We’re talking about a living organism which governments have taken upon themselves to designate as an illegal substance. Despite no existing evidence of anyone ever dying of a marijuana overdose, possession of this plant is still illegal in many parts of the world.
Marijuana has been found to suppress cancer, reduce blood pressure, treat glaucoma, alleviate pain and even inhibit HIV. It is an antioxidant, anti-inflammatory and neuroprotective. Can you understand more now why it’s illegal?
No Independent Study Has Ever Linked Marijuana to Psychosocial Problems
“Currently, there is no strong evidence that use of cannabis of itself causes psychological or social problems,” such as mental illness or school failure, lead study author Dr. John Macleod of the University of Birmingham in the UK told Reuters Health. “There is… evidence that cannabis use is associated with these things, but this association could have several explanations,” he said, citing factors such as adversity in early life, which may itself be associated with cannabis use and psychosocial problems.
Macleod and his team reviewed 48 long-term studies, 16 of which provided the highest quality information about the association between illicit drug use reported by people 25 years old or younger and later psychological or social problems. Most of the drug-specific results involved cannabis use. Cannabis use was not consistently associated with violent or antisocial behavior, or with psychological problems.
Notably, recent studies have shown CBD, a compound in cannabis, to be an effective atypical anti-psychotic in treating schizophrenia, a disease many other studies have inconsistently claimed cannabis to cause.
In another study, Scientists from King’s College, London, found occasional pot use could actually improve concentration levels. The study, carried in the American Journal of Epidemiology, tested the mental function and memory of nearly 9,000 Britons at age 50 and found that those who had used illegal drugs as recently as in their 40s did just as well, or slightly better, on the tests than peers who had never used drugs.
“Overall, at the population level, the results seem to suggest that past or even current illicit drug use is not necessarily associated with impaired cognitive functioning in early middle age,” said lead researcher Dr Alex Dregan.
Dr Dregan’s team used data on 8,992 42-year-olds participating in a UK national health study, who were asked if they had ever used any of 12 illegal drugs. Then, at the age of 50, they took standard tests of memory, attention and other cognitive abilities. Overall, the study found, there was no evidence that current or past drug users had poorer mental performance. In fact, when current and past users were lumped together, their test scores tended to be higher.
The Age of Deception is Ending
In 2003, the U.S. Government as represented by the Department of Health and Human Services filed for, and was awarded a patent on cannabinoids. The reason? Because research into cannabinoids allowed pharmaceutical companies to acquire practical knowledge on one of the most powerful antioxidants and neuroprotectants known to the natural world.
The U.S. Patent 6630507 was specifically initiated when researchers found that cannabinoids had specific antioxidant properties making them useful in the treatment and prophylaxis of wide variety of oxidation associated diseases, such as ischemic, age-related, inflammatory and autoimmune diseases. The cannabinoids are found to have particular application as neuroprotectants, for example in limiting neurological damage following ischemic insults, such as stroke and trauma, or in the treatment of neurodegenerative diseases, such as Alzheimer’s disease, Parkinson’s disease and HIV dementia. Nonpsychoactive cannabinoids, such as cannabidiol, are particularly advantageous to use because they avoid toxicity that is encountered with psychoactive cannabinoids at high doses useful in the method of the present invention.
Now, as more and more people around the world are waking up to the health benefits of cannabis, it is increasingly being legalized for medical and even recreational use. Although this increased awareness comes with some unique challenges, it also offers an amazing opportunities to further educate millions more people on the health benefits of marijuana.
It’s no surprise that the United States has decreed that marijuana has no accepted medical use and should remain classified as a highly dangerous “Schedule I” drug, like heroin. Accepting and promoting the powerful health benefits of marijuana would instantly cut huge profits geared towards cancer treatment and the U.S. would have to admit it imprisons the population for no cause. Nearly half of all drug arrests in the United States are for marijuana.
According to MarijuanaNews.com editor Richard Cowan, the answer is because it is a threat to cannabis prohibition: “There really is massive proof that the suppression of medical cannabis represents the greatest failure of the institutions of a free society, medicine, journalism, science, and our fundamental values,” Cowan notes.
Top Health Benefits of Marijuana
1. Cancer
Cannabinoids, the active components of marijuana,inhibit tumor growth in laboratory animals and also kill cancer cells. Western governments have known this for a long time yet they continued to suppress the information so that cannabis prohibition and the profits generated by the drug industry proliferated.
THC that targets cannabinoid receptors CB1 and CB2 is similar in function to endocannabinoids, which are cannabinoids that are naturally produced in the body and activate these receptors. The researchers suggest that THC or other designer agents that activate these receptors might be used in a targeted fashion to treat lung cancer.
2. Tourette’s Syndrome
Tourette’s syndrome is a neurological condition characterized by uncontrollable facial grimaces, tics, and involuntary grunts, snorts and shouts.
Dr. Kirsten Mueller-Vahl of the Hanover Medical College in Germany led a team that investigated the effects of chemicals called cannabinols in 12 adult Tourette’s patients. A single dose of the cannabinolproduced a significant reduction in symptoms for several hours compared to placebo, the researchers reported.
3. Seizures
Marijuana is a muscle relaxant and has “antispasmodic” qualities that have proven to be a very effective treatment for seizures. There are actually countless cases of people suffering from seizures that have only been able to function better through the use of marijuana.
4. Migraines
Since medicinal marijuana was legalized in California, doctors have reported that they have been able to treat more than 300,000 cases of migraines that conventional medicine couldn’t through marijuana.
5. Glaucoma
Marijuana’s treatment of glaucoma has been one of the best documented. There isn’t a single valid study that exists that disproves marijuana’s very powerful and popular effects on glaucoma patients.
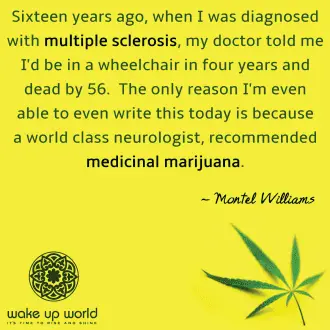 6. Multiple Sclerosis
6. Multiple Sclerosis
Marijuana’s effects on multiple sclerosis patients became better documented when former talk-show host, Montel Williams began to use pot to treat his MS. Marijuana works to stop the neurological effects and muscle spasms that come from the fatal disease.
7. ADD and ADHD
A well documented USC study done about a year ago showed that marijuana is not only a perfect alternative for Ritalin but treats the disorder without any of the negative side effects of the pharmaceutical.
8. IBS and Crohn’s
Marijuana has shown that it can help with symptoms of the chronic diseases as it stops nausea, abdominal pain, and diarrhea.
9. Alzheimer’s
Despite what you may have heard about marijuana’s effects on the brain, the Scripps Institute, in 2006, proved that the THC found in marijuana works to prevent Alzheimer’s by blocking the deposits in the brain that cause the disease.
10. Premenstrual Syndrome
Just like marijuana is used to treat IBS, it can be used to treat the cramps and discomfort that causesPMS symptoms. Using marijuana for PMS actually goes all the way back to Queen Victoria.
Other Benefits
In addition to the 10 health benefits detailed above, findings published in the journal PLoS ONEindicate researchers have now have discovered that marijuana-like chemicals trigger receptors on human immune cells that can directly inhibit a type of human immuno-deficiency virus (HIV) found in late-stage AIDS.
Further research has also shown cannabinoids can reduce the risk of heart attacks by 66% and reduce insulin dependent diabetes by 58%.
Mounting Evidence Suggests Raw Cannabis is Best
Cannabis clinician Dr. William Courtney recommends drinking 4 – 8 ounces of raw flower and leaf juice from any Hemp plant, 5 mg of Cannabidiol (CBD) per kg of body weight, a salad of Hemp seed sprouts and 50 mg of THC taken in 5 daily doses.
Why raw? Heat destroys certain enzymes and nutrients in plants. Incorporating raw cannabis allows for a greater availability of those elements. Those who require large amounts of cannabinoids without the psychoactive effects need to look no further than raw cannabis. In this capacity, it can be used at 60 times more tolerance than if it were heated.
Raw cannabis is considered by many experts as a dietary essential. As a powerful anti-inflammatory and antioxidant, raw cannabis may be right up there with garlic and turmeric.
Article sources:
About the author:
Marco Torres is a research specialist, writer and consumer advocate for healthy lifestyles. He holds degrees in Public Health and Environmental Science, and is a professional speaker on topics such as disease prevention, environmental toxins and health policy.
Recommended reading from Marco Torres:
- Hemp Can Free Us From Oil, Prevent Deforestation and Cure Cancer – So Why Is It Illegal?
- The Endocannabinoid System and How THC Cures Cancer
- Cannabis Infused Coffee – Consumers Grow Wise to Health Benefits of Marijuana
- Cannabis Oil Cures Infant of Cancer, Dissolves Inoperable Tumor
- 5 Reasons to Juice Rather Than Smoke Cannabis
- Study Shows The Therapeutic Effects of Marijuana on Autistic Children
- 5 Diseases Proven To Respond Better To Cannabis Than Prescription Drugs
- Cannabis-Based Batteries Could Change the Way We Store Energy Forever
- Another Reason Marijuana is Illegal: It Prevents the Spread of HIV
- 4 Diseases That Can Be Reversed Naturally Without Pharmaceutical Drugs
- Woman Shrinks Inoperable Mass, Heals Her Thyroid Disease With Cannabis Oil
- The Top 15 Lies You’re Being Told About Health and Mainstream Medicine
- Mexico Rules Consumption and Cultivation of Cannabis is a Fundamental Human Right
Please note: This article originally appeared on PreventDisease.com, reproduced with permission.
Friday, December 29, 2017
Healing Properties of Apples
The Amazing Healing Properties of Apples
Posted on: Thursday, December 28th 2017 at 11:00 am
Written By: Sayer Ji, Founder
This article is copyrighted by GreenMedInfo LLC, 2017
This commonly overlooked superfood protects the body from nuclear fallout, kills a wide range of cancers, and keeps the arteries unclogged -- to name but a few, experimentally confirmed ways in which the apple awakens your inner physician.
"An apple a day keeps the doctor away."
This age old saying has never rang truer with greater promise and authority than it does today. As in the modern era, doctors bring with them a battery of tests, drugs, and interventions, all of which carry unintended, adverse health risks that often outweigh their purported benefits, and are therefore best avoided whenever possible.
While some might take this opening aphorism as mere folk medicine fantasy, the reality is that the medicinal properties of apple are well-documented within the biomedical literature.
For instance, apple consumption has been the subject of quite a few studies on colorectal cancer risk reduction. [i] [ii] [iii] Other cancers that apple constituents have been studied to kill in pre-clinical research include:
- Liver Cancer: apple juice, apple pectin and apple peel has been experimentally confirmed to kill liver cancer,[iv]
- Breast Cancer: apples have been found to both prevent and to suppress mammary cancers in the animal model.[v]
- Multi-Drug Resistant Cancer: carotenoids extracted from apple have been found to inhibit drug resistant cancer cell line proliferation.[vi]
- Esophageal Cancer: An apple-derived procyanidin has been found to suppress esophageal cancer. [vii]
- Stomach Cancer: One of the ways in which apple constituents prevent stomach cancer is through their inhibition of Helicobacter pylori, one of the main infectious agents linked to both ulcer and gastric cancer.[viii] But apple procyanidin has also been studied for its ability to directly induce programmed cell death within stomach cancer cells.[ix]
It is likely that many of the fundamental processes involved in cancer initiation and promotion are inhibited by apples and their constituents, and therefore apples may protect against far more cancers than referenced above. It appears that no matter what part of apple is studied, it has anti-tumor properties. Apple cider vinegar, for instance, has been found to contain an anti-tumor compound which results from the acetic acid fermentative process known as alpha-glycan.
Another proven way in which apples reduce the risk of cancer is through their ability to remove carcinogenic radioisotopes that have accumulated in our bodies as a result of the fallout from nuclear weapons, depleted uranium munitions, and nuclear energy and disaster-associated pollution, e.g. Chernobyl and Fukushima.
Post-Chernobyl, for instance, apple pectin was used to reduce Cesium-137 levels in exposed children, in some cases by over 60%.[x] From 1996 to 2007, a total of more than 160,000 "Chernobyl" children received pectin food additives. As a result, levels of Cs-137 in children's organs decreased after each course of pectin additives by an average of 30-40%.[xi] Significant reductions were noted in as short a time period as 16 days.[xii] Apple pectin has even been found to prevent the most deadly, and entirely man-made radioisotope, Plutonium-239, from absorbing in the gastrointestinal tract of animals fed it.[xiii]
We could, therefore, modernize our apple aphorism by saying "an apple a day keeps the nuclear fallout away." And truly, there are very few other substances, natural or synthetic, that have ever been found to protect against plutonium exposure. Apples, therefore, are truly super-foods in this respect.
Other noteworthy "evidence-based" medicinal properties of apple include:
- Diarrhea: Apple, in combination with chamomile, shortens the course of unspecific diarrhea in children.[xiv]
- Hardening of the Arteries (Atherosclerosis): Preclinical research indicates that apple contains compounds which prevent the formation of plaque within the arteries.[xv] One rabbit study, for instance, found that apple juice was capable of preventing the progression of atherosclerosis in a high cholesterol diet induced model of atherosclerosis.[xvi]
- Overweight: A human study found significant weight loss associated with a daily intake of three apples or three pears among overweight women.[xvii]
- Anti-Aging (Brain): Apples have been found to prevent oxidative damage and impaired maze performance,[xviii]as well as decreases in cognitive performance in aging mice.[xix] Also, a study performed on mice found that apple juice actually reduced the production of pathological amyloid-beta levels (associated with Alzheimer's disease) in the mouse brain.[xx]
- Bowel Inflammation: Preclinical research has found that apple procyanidins [xxi]reduces bowel inflammation.[xxii]
- Vaccine-Induced Toxicity: Many natural substances, including breast milk, have been found to decrease the synthetically-produced immune reaction associated with vaccines, and their adjuvants. Apple polyphenol counts among these, and has been found to prevent cholera toxin when used as an immune stimulant within vaccines from doing as much damage than it would otherwise do.
- Periodontal Disease: We all know the sensation that follows eating an apple – that astringent property, where our gums feel squeaky clean. This is due, in part, to quercetin, which is found in apples, tea and onions, for example. It bears significant antimicrobial properties.[xxiii] Apple polyphenol also protects against periodontal ligament cell destruction associated with Porphyromonas gingivalis, a pathogenic anaerobic bacteria, infection.[xxiv]
- Advanced Glycation End-products (AGEs): AGEs are associated with the oxidation of blood sugars, primarily. These sugars becomes caramelized when exposed to oxidants, and then binds to cell structures, e.g. fats/proteins, causing damage. Apple leaves have been found to have significant anti-AGE activity, including the vasoconstriction associated with AGE-induced endothelial dysfunction.[xxv]
- Hair Loss: Remarkably, a procyanidin, labeled B-2, from apples promotes hair growth, in the cell model.[xxvi]
- Staphylococcal Infections: Apple pectin has been shown to inhibit synthesis of types A and B staphylococcal enterotoxins, which can cause profound bodily damage.[xxvii]
- Influenza Infection: Over 60 years ago researchers found that the complex carbohydrates that make up apple pectin inhibit the infectivity of influenza A virus in chicken blood, as well in embryonated eggs, indicating its potential anti-influenza properties.[xxviii]
The list of evidence-based therapeutic properties of apple is rather extensive. To view the full range of experimentally confirmed benefits view them here: Apple's Health Benefits.
Ultimately, this research on apples indicates how important whole foods are to our overall health. Apples are not medicine, rather, they are the means by which medicines become unnecessary. It is through authentic nourishment and detoxification – both functions which are provided to us through most fruits - that we prevent and treat disease (note: these statements likely will never be evaluated or approved by the FDA, because they are true). Also, fruit are archetypally beneficial foods for the human species; we have indexed over 300 experimentally confirmed health benefits of fruit on our database so far. Our evolutionary legacy (confirmed through modern genetic testing*) indicates that our pre-human ancestors lived in a jungle setting, where fruit would have been available year round.
This would, in fact, explain why we no longer synthesize vitamin c from glucose – we were so "spoiled" by the abundance of fruit available for so long that we gave up (via genetic mutation or atavism) our ability to provide it to ourselves. Plants and animals live in symbiosis. For the same reason that our lungs take in oxygen and give off carbon dioxide (which is live-giving to plants), the fruits of these same plants provide a seed (which we help disperse), and a flesh to entice us to consume it. Fruit, therefore, is a food source that is as ancient as human origins itself. Could this be one reason why apples seem capable of these amazing feats of healing? Perhaps.
Next time you crunch into a crisp, fresh, organic apple, consider all that it has to offer, not theoretically, but viscerally. Experience the joy (the word fruit, etymologically, comes from the Latin word frui, meaning ENJOY), on a first hand basis. Also, if you have never done an apple mono-diet before, consider it. It is not so much a fruit fast, as a feast. Grab a bag of organic apples, and whenever you are hungry eat one. You will be surprised by how immediate you are satiated, and how cleansing and liberating on the body the exclusive consumption of such a simple, perfect food like the apple really is. One can easily go a day or two using this approach, often with the result of feeling completely renewed and refreshed.
Resources
*Note: It is a little known and under-appreciated fact that all humans are born with a serious, life-threatening genetic defect: namely, the inability to manufacture Vitamin C.
This defect occurred approximately 63 million years ago, when our haplorrhini ("simple nosed") primate predecessors lost the gene (Gulnolactone oxidase pseudogene – GULOP), responsible for the manufacture of Vitamin C from glucose.
The ability to synthesize Vitamin C, in fact, has been lost several times in vertebrates, e.g. in guinea pigs, some bats, some fishes, passeriform birds and in primates of the suborder Haplorrhini, which includes monkes, apes and humans.
- [i] Wieslaw Jedrychowski, Umberto Maugeri. An apple a day may hold colorectal cancer at bay: recent evidence from a case-control study. Rev Environ Health. 2009 Jan-Mar;24(1):59-74. PMID: 19476292
- [ii] Wieslaw Jedrychowski, Umberto Maugeri, Tadeusz Popiela, Jan Kulig, Elzbieta Sochacka-Tatara, Agnieszka Pac, Agata Sowa, Agnieszka Musial. Case-control study on beneficial effect of regular consumption of apples on colorectal cancer risk in a population with relatively low intake of fruits and vegetables. Basic Clin Pharmacol Toxicol. 2009 Mar;104(3):262-71. Epub 2009 Jan 20. PMID: 19926998
- [iii] H Deneo-Pellegrini, E De Stefani, A Ronco. Vegetables, fruits, and risk of colorectal cancer: a case-control study from Uruguay. Nutr Cancer. 1996;25(3):297-304. PMID: 8771572
- [iv] GreenMedInfo.com, Apple's Anti-Liver Cancer Properties
- [v] GreenMedInfo.com, Apple's Anti-Breast Cancer Properties
- [vi] Péter Molnár, Masami Kawase, Kazue Satoh, Yoshitaka Sohara, Toru Tanaka, Satoru Tani, Hiroshi Sakagami, Hideki Nakashima, Noboru Motohashi, Nóra Gyémánt, Joseph Molnár. Biological activity of carotenoids in red paprika, Valencia orange and Golden delicious apple. Phytother Res. 2005 Aug;19(8):700-7. PMID: 16177974
- [vii] Roberto Pierini, Paul A Kroon, Sylvain Guyot, Kamal Ivory, Ian T Johnson, Nigel J Belshaw. Procyanidin effects on oesophageal adenocarcinoma cells strongly depend on flavan-3-ol degree of polymerization. Mol Nutr Food Res. 2008 Dec;52(12):1399-407. PMID: 18683822
- [viii] GreenMedInfo.com, Helicobacter Pylori and Apples
- [ix] Hiroshige Hibasami, Toshihiko Shohji, Ichirou Shibuya, Kazuko Higo, Tomomasa Kanda. Induction of apoptosis by three types of procyanidin isolated from apple (Rosaceae Malus pumila) in human stomach cancer KATO III cells. Int J Mol Med. 2004 Jun;13(6):795-9. PMID: 15138614
- [x] V B Nesterenko, A V Nesterenko, V I Babenko, T V Yerkovich, I V Babenko. Reducing the 137Cs-load in the organism of "Chernobyl" children with apple-pectin. Swiss Med Wkly. 2004 Jan 10;134(1-2):24-7. PMID: 14745664
- [xi] Vassily B Nesterenko, Alexey V Nesterenko. 13. Decorporation of Chernobyl radionuclides. Phytother Res. 2009 Apr;23(4):564-71. PMID: 20002057
- [xii] G S Bandazhevskaya, V B Nesterenko, V I Babenko, T V Yerkovich, Y I Bandazhevsky. Relationship between caesium (137Cs) load, cardiovascular symptoms, and source of food in 'Chernobyl' children -- preliminary observations after intake of oral apple pectin. Swiss Med Wkly. 2004 Dec 18;134(49-50):725-9. PMID: 15635491
- [xiii] V S Kalistratova, G A Zalikin, P G Nisimov, I B Romanova. [Study of the effect of a food additive Medetopect on metabolic kinetics of transuranic radionuclides in animal body]. Radiats Biol Radioecol. 1998 Jan-Feb;38(1):35-41. PMID: 9606404
- [xiv] Brigitta Becker, Ulrike Kuhn, Bettina Hardewig-Budny. Double-blind, randomized evaluation of clinical efficacy and tolerability of an apple pectin-chamomile extract in children with unspecific diarrhea. Arzneimittelforschung. 2006;56(6):387-93. PMID: 16889120
- [xv] GreenMedInfo.com, Apple's Anti-Atherosclerosis Properties
- [xvi] Mahbubeh Setorki, Sedighe Asgary, Akram Eidi, Ali Haeri Rohani, Nafiseh Esmaeil. Effects of apple juice on risk factors of lipid profile, inflammation and coagulation, endothelial markers and atherosclerotic lesions in high cholesterolemic rabbits. Lipids Health Dis. 2009;8:39. Epub 2009 Oct 5. PMID: 19804641
- [xvii] Maria Conceição de Oliveira, Rosely Sichieri, Anibal Sanchez Moura. Weight loss associated with a daily intake of three apples or three pears among overweight women. Nutrition. 2003 Mar;19(3):253-6. PMID: 12620529
- [xviii] Flaubert Tchantchou, Amy Chan, Lydia Kifle, Daniela Ortiz, Thomas B Shea. Apple juice concentrate prevents oxidative damage and impaired maze performance in aged mice. Ann Clin Psychiatry. 2009 Jul-Sep;21(3):148-61. PMID: 16340085
- [xix] [No authors listed]. Apple juice concentrate maintains acetylcholine levels following dietary compromise. J Alzheimers Dis. 2006 Aug;9(3):287-91. PMID: 16914839
- [xx] Amy Chan, Thomas B Shea. Dietary supplementation with apple juice decreases endogenous amyloid-beta levels in murine brain. Int J Mol Med. 2010 Oct;26(4):447-55. PMID: 19158432
- [xxi] Naoto Yoshino, Kohtaro Fujihashi, Yukari Hagiwara, Hiroyuki Kanno, Kiyomi Takahashi, Ryoki Kobayashi, Noriyuki Inaba, Masatoshi Noda, Shigehiro Sato . Co-administration of cholera toxin and apple polyphenol extract as a novel and safe mucosal adjuvant strategy. Vaccine. 2009 Jul 30;27(35):4808-17. Epub 2009 Jun 17. PMID: 19539583
- [xxii] GreenMedInfo.com, Apples and Bowel Inflammation
- [xxiii] F Geoghegan, R W K Wong, A B M Rabie. Inhibitory effect of quercetin on periodontal pathogens in vitro. Phytother Res. 2009 Dec 2. Epub 2009 Dec 2. PMID: 19957242
- [xxiv] Hiroaki Inaba, Motoyuki Tagashira, Tomomasa Kanda, Takashi Ohno, Shinji Kawai, Atsuo Amano. Apple- and hop-polyphenols protect periodontal ligament cells stimulated with enamel matrix derivative from Porphyromonas gingivalis. J Periodontol. 2005 Dec;76(12):2223-9. PMID: 16332233
- [xxv] Thomas Dugé de Bernonville, Sylvain Guyot, Jean-Pierre Paulin, Matthieu Gaucher, Laurent Loufrani, Daniel Henrion, Séverine Derbré, David Guilet, Pascal Richomme, James F Dat, Marie-Noëlle Brisset . Dihydrochalcones: Implication in resistance to oxidative stress and bioactivities against advanced glycation end-products and vasoconstriction. Phytochemistry. 2009 Dec 18. Epub 2009 Dec 18. PMID: 20022617
- [xxvi] A Kamimura, T Takahashi. Procyanidin B-2, extracted from apples, promotes hair growth: a laboratory study. Sci Total Environ. 2010 Feb 13. Epub 2010 Feb 13. PMID: 11841365
- [xxvii] F S Fluer, D D Men'shikov, E B Lazareva, V Ia Prokhorov, A V Vesnin. [Influence of various pectins on production of staphylococcal enterotoxins types A and B]. Zh Mikrobiol Epidemiol Immunobiol. 2007 Nov-Dec(6):11-6. PMID: 18277535
- [xxviii] R H Green, D W Woolley. INHIBITION BY CERTAIN POLYSACCHARIDES OF HEMAGGLUTINATION AND OF MULTIPLICATION OF INFLUENZA VIRUS. J Exp Med. 1947 Jun 30;86(1):55-64. PMID: 19871655
Sayer Ji is founder of Greenmedinfo.com, a reviewer at the International Journal of Human Nutrition and Functional Medicine, Co-founder and CEO of Systome Biomed, Vice Chairman of the Board of the National Health Federation, Steering Committee Member of the Global Non-GMO Foundation.
Disclaimer: This article is not intended to provide medical advice, diagnosis or treatment. Views expressed here do not necessarily reflect those of GreenMedInfo or its staff.
Internal Site Commenting is limited to members.
Disqus commenting is available to everyone.
To comment:
Wednesday, December 27, 2017
Skip Microwaved Eggs
Skip Microwaved Eggs
|
|
Story at-a-glance
- Eggs are close to being a perfect food, full of vitamins A, D, E, K and B12, omega-3 fats, folate and antioxidants; they are versatile, kids love them and they can be cooked in a variety of ways
- Reheating hard-boiled eggs in a microwave oven may superheat the yolk, triggering a loud explosion, and may burn your face, eyes and mouth
- Microwave ovens cause chemical changes in your food that reduce nutrition, and use microwave electromagnetic fields that disrupt mitochondrial function and increase your risk for negative health conditions
- Purchasing farm-fresh, organic, free-range pastured eggs delivers the best nutrition, and cooking them the least amount of time delivers the most antioxidant and vitamin benefits
By Dr. Mercola
Eggs are close to being a perfect food. Egg yolks deliver vitamins A, D, E, K and B12, omega-3 fats, folate and antioxidants. They are also versatile. You can use them at any meal, kids love them and they can be cooked inside or outside the shell.
Until the 1920s, chickens were raised almost exclusively for their ability to lay eggs. The meat was seasonally available, expensive and not very tasty.1 This changed, quite by accident, in 1923 when farm wife Cecile Steele mistakenly ordered 500 hatchlings instead of 50. The farmer sold the extra chickens for meat. The "mistake" was so successful, she repeated it in the following years. Then, in 1948 a contest was sponsored to breed a better tasting chicken and today Americans eat more chicken than they did in the early 20th century.2
In the 1960s, as the low-fat fad gained momentum, doctors recommended eating just the whites of eggs as the yolks were reportedly high in cholesterol, which was mistakenly thought to be bad for your health. Media warned eggs increased your cholesterol level and your risk of heart disease.
Today, following the recommendations of researchers and scientists, the egg is recognized as a nutritious food and the U.S. Government Office of Disease Prevention and Heath Promotion's Dietary Guidelines for Americans3 2015-2020 has dropped their strict limits on dietary cholesterol.4 Although eggs offer significant nutritional benefits, it is vital to seek out high quality eggs and protect your health from cooking methods that may trigger significant burns or create toxins in your food.5
Superheating in a Microwave Is Explosive
Hard-boiled eggs, reheated in a microwave, are an accident waiting to happen. A 9-year-old girl in the U.K. found that out when she reheated an egg for 40 seconds, and while carrying the egg to a table, the egg exploded.6 Pieces from the superheated egg tore her cornea and required a lens replacement to restore her vision months later.
Ophthalmologists used this as a case study when they made an appeal to microwave manufacturers to place warning labels on microwave ovens about the dangers of exploding eggs.7 Manufacturers warn against microwaving eggs without first piercing them several times. But those warnings are found in leaflets that accompany the microwave, which many owners toss, explains Dr. Saurabh Goyal, ophthalmologist at Queen Mary's Hospital in the U.K and one of the letter's authors.8
It is not just eggs that explode in the microwave. An Illinois woman scalded her face and corneas after a bowl of water she heated in the microwave exploded in her face.9 Louis Bloomfield, Ph.D., a University of Virginia physicist explained to ABC News:
"You're used to having water or liquid boil when you heat it above a certain temperature, but there are occasions, and they're more frequent than you'd expect, in a microwave oven when the water goes to or above boiling without any bubbles forming. And that's a phenomenon known as superheating. Well, it's almost like a bomb once you've got it superheated adequately, because anything that triggers the boiling, once you've reached that temperature, will cause catastrophic, very sudden flash boiling."
A review of the literature published in 2001 found 13 cases where individuals were burned by exploding eggs after they were removed from a microwave oven.10 In some of those cases the explosion occurred even after the shell or yolk had been pierced. In 2002, an estimated 2,700 people in the U.K. sustained a microwave-related injury, half of those from hot liquid. More recently, a lawsuit was filed after a customer at a restaurant bit into an egg that had been reheated in a microwave. The egg exploded in his mouth with a loud bang, causing burns.
Exploding Eggs Do Not Cause Acoustical Damage
During the ensuing court case, a San Francisco-based firm specializing in acoustics was asked to determine if the noise from the exploding egg could have caused hearing damage.11 The firm presented their results during the 174 Meeting of the Acoustical Society of America.
During the experiments, the scientists controlled variables, including measurement of sound levels, internal temperature of the eggs and documentation of the different kinds and sizes of the eggs used.12 hard-boiled eggs were put into a water bath and heated for three minutes in the microwave. The temperature of the water bath was measured in the middle and end of the heating time.
The eggs were then removed from the water bath, placed on the floor and pierced with a fast-acting meat thermometer to both pierce the egg and measure the internal temperature of the yolk. The researchers found the internal temperature was consistently higher than the water bath from which the eggs had been removed. This suggested to the researchers that the egg was more receptive to heating from the microwave than was the surrounding water. The scientists hypothesized:13
"... that the egg's protein matrix traps small pockets of water within the yolk, causing the pockets to superheat well above the nominal boiling temperature of ordinary tap water. When these superheated pockets are disturbed by a penetrating device, or if one attempts to bite into the egg yolk, the water pockets all boil in a furious chain reaction leading to an explosion-like phenomenon."
The team was tasked to answer the question of whether an exploding egg created enough pressure to damage hearing. They found that, although loud, a single explosion wasn't enough to damage hearing. Anthony Nash, currently serving on a U.S. Technical Advisory Group to review and comment on international standards addressing mechanical vibration in the environment, explains their results:
"We needed to quantify the peak sound pressures from an exploding egg so we could compare it to hearing damage risk criteria. At 1 foot away, the peak sound pressure levels from microwaved eggs covered a wide range from 86 up to 133 decibels.
Only 30 percent of the tested eggs survived the microwave heating cycle and exploded when pierced by a sharp object. On a statistical basis, the likelihood of an egg exploding and damaging someone's hearing is quite remote. It's a little bit like playing egg roulette."
Chemical Changes Produce Toxins and Reduce Nutritional Benefits
While the probability of hearing loss may be remote, the likelihood of chemical changes in food cooked in a microwave is far higher. Microwaving alters the food's chemical structure and begins in areas with the highest water concentration. As water is not uniformly present throughout your food, it is frequently unevenly heated. Knowledge of the changes to food from microwave heating has dramatically increased from the time the appliance was first introduced.
For example, using any type of plastic container opens up the probability that chemicals like BPA will leach into the food, contaminating it with hormone disrupting chemicals. High heat, such as in microwave ovens, may also produce heterocyclic amines (HCAs), polycyclic aromatic hydrocarbons (PAHs) and advanced glycation end products (AGEs), each of which are known carcinogens.14
Research into nutritional changes related to thawing, cooking or reheating foods in a microwave is slowly demonstrating that altering the chemical structure of food using microwave radiation likely also damages nutrients. One study found microwaved broccoli lost up to 97 percent of beneficial antioxidants,15 while as little as 60 seconds inactivated all the allinase in garlic, the active ingredient against cancer.16
A Scandinavian study found microwaving asparagus reduced vitamin C17 and a Japanese study found six minutes of heating rendered up to 40 percent of B12 in milk inert.18 Researchers have also discovered microwaves cause a higher degree of "protein unfolding" than conventional heating19 and will destroy essential disease-fighting agents in breast milk that help protect your baby.20 For this reason, and because microwaving may cause the milk to get excessively hot and may burn your baby, NEVER heat breast milk in the microwave.
Microwave Radiation Triggers Massive Mitochondrial Dysfunction
An error occurred.
Try watching this video on www.youtube.com, or enable JavaScript if it is disabled in your browser.
Microwave radiation is a form of electromagnetic field (EMF) radiation that is common to cellphones, Wi-Fi routers and microwave ovens. EMFs are a pernicious health hazard that affects your body at the cellular level, causing massive mitochondrial dysfunction through free radicals from peroxynitrite. This short video with Martin Pall, Ph.D., is an introduction to an hourlong interview where we discuss the damage EMF triggers.
Pall has identified and published research describing the likely molecular mechanisms of how EMFs damage plants, animals and humans.21,22,23,24 His research demonstrates exposure to EMF radiation opens voltage-gated calcium channels in your cells’ membranes, allowing a massive influx of calcium into your cells.
Excess intracellular calcium increases calcium signaling and increases nitric oxide (NO) to massively excessive amounts that interact with superoxide. While lower amounts of NO have beneficial health effects, larger quantities trigger a reaction that forms peroxynitrite, an extremely potent oxidant stressor.
It is important to state that not all oxidative stress is harmful. Your body requires a baseline of free radicals for optimal health. NO, for example, is a free radical that has several beneficial effects when produced in moderation. NO helps reduce your blood pressure, support your immune system and naturally reduces platelet aggregation that reduces your risk for heart attack and stroke. The problem occurs with excessive oxidative stress that can be triggered by exposure to microwave EMF radiation.
Nutrition in the Egg Is Dependent on How the Chicken Was Raised
As with most biological processes, the end result is a culmination of what was used to build the organism. In the case of eggs, there is a vast nutritional difference between chickens raised in concentrated animal feeding operations (CAFOs) and fed GE grains supplemented with vitamins and antibiotics — standard supermarket eggs — and organic, free-range pastured eggs.
You'll be able to tell if your eggs are free-range or pastured by the color of the yolk. Hens allowed to forage in a pasture produce eggs with rich orange colored yolks, while caged hens produce eggs with pale, anemic yellow yolks.
The Cornucopia Institute addresses some of the issues of nutritional value in eggs in their egg report25 and scorecard26 that ranks egg producers according to 28 organic criteria. This information may help you make a more educated choice when buying eggs at the supermarket. Ultimately, your best choice is to purchase your eggs and grass fed meat directly from a trusted local farmer.
Alternatively, you might consider raising your own backyard chickens. This practice is growing in popularity and many U.S. cities are adjusting their zoning restrictions accordingly. Requirements vary depending upon your locale, with some limiting the number you can raise or requiring a quarterly inspection and permits (at a cost). Check with your city, but you may be surprised to learn they already allow chickens. If you don't want to raise your own chickens, but still want farm-fresh eggs, you have options.
If you live in an urban area, visiting the local health food stores is typically the quickest route to finding high-quality local egg sources. Farmers markets and food co-ops are another great way to meet the people who produce your food. With face-to-face contact, you can get your questions answered and know exactly what you're buying. Better yet, visit the farm — ask for a tour. If they have nothing to hide, they should be eager to show you their operation.
The Choline Connection
Eggs are one of the best nutritional sources of choline available. Choline helps to keep your cell membranes functioning, plays a role in communication in your nervous system and reduces chronic inflammation. Your body uses it to make acetylcholine, used in your brain to store memories. During pregnancy, a woman's body uses it to prevent birth defects and plays a role in brain development.
However, as important as this nutrient is to your health, research finds only 8 percent of American adults are consuming enough.27 Researchers have found it's "extremely difficult" to get enough choline unless you eat eggs or take a dietary supplement. Of those who do eat eggs regularly, more than 57 percent met adequate intake levels, compared to 2.4 percent who don't eat eggs.
Some of the symptoms of low levels are similar to early symptoms of dementia or of menopause, and include memory problems, lethargy and persistent brain fog. Since your body can only synthesize small amounts at a time, it's necessary to routinely get it from your diet.
Healthiest Way to Eat Eggs
Although versatile, how you cook them may lower the antioxidants available. According to one study,28 storing eggs in the refrigerator didn't change the nutrient values, but boiling and frying significantly reduced oxygen radical absorbance capacity (ORAC) value (a test that attempts to quantify the total antioxidant capacity) and the contents of free amino acid, lutein and zeaxanthin.
In another review of the nutrient value, cooking reduced vitamin A content between 17 percent and 20 percent.29 Overall, the shorter the amount of time spent cooking eggs, the more nutritional benefits they retain. Soft boiling or poaching until firm are good ways of cooking within those parameters. However, the healthiest way to consume eggs when they are from a high-quality source of pastured, organic hens, is raw.
When eggs are baked for 40 minutes they can lose as much as 61 percent of vitamin D content, compared to 18 percent when they're boiled or fried for a shorter period.30 Another study reported that consumption of antioxidants is known to reduce oxidative damage in cells and improve health. In addition to well-known nutritional contributions, eggs play an important role as an antioxidant food.31
Subscribe to:
Posts (Atom)